Up To The Minute Health Plan Finance And Risk Management AHM-520 Exam Prep
We provide real AHM-520 exam questions and answers braindumps in two formats. Download PDF & Practice Tests. Pass AHIP AHM-520 Exam quickly & easily. The AHM-520 PDF type is available for reading and printing. You can print more and practice many times. With the help of our AHIP AHM-520 dumps pdf and vce product and material, you can easily pass the AHM-520 exam.
AHIP AHM-520 Free Dumps Questions Online, Read and Test Now.
NEW QUESTION 1
In order to print all of its forms in-house, the Prism health plan isconsidering the purchase
of 10 new printers at a total cost of $30,000. Prismestimates that the proposed printers have a useful life of 5 years. Under itscurrent system, Prism spends $10,000 a year to have forms printed by a localprinting company. Assume that Prism selects a 15% discount rate based onits weighted-average costs of capital. The cash inflows for each year,discounted to their present value, are shown in the following chart: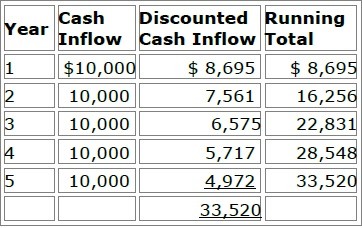
Prism will use both the payback method and the discounted payback methodto analyze the worthiness of this potential capital investment. Prism's decisionrule is to accept all proposed capital projects that have payback periods offour years or less.
Now assume that Prism decides to use the net present value (NPV) method toevaluate this potential investment's worthiness and that Prism will accept theproject if the project's NPV is greater than $4,000. Using the NPV method,Prism would correctly conclude that this project should be
- A. Rejected because its NPV is $3,520
- B. Accepted because its NPV is $5,028
- C. Accepted because its NPV is $16,480
- D. Accepted because its NPV is $23,520
Answer: A
NEW QUESTION 2
The following statements are about rate ratios used by health plans. Select the answer choice containing the correct statement:
- A. While rate ratios consider family size, they are most often based on competitive factors, such as the ratios being used by competitors and the ratios that plan sponsors are requesting.
- B. If the rate ratio for a couple rate category is 2.0, then the single premium is divided by 2.0 to derive the couple rate category premium.
- C. A rate ratio can only be increased if the health plan has obtained regulatory approval.
- D. The effect of a typical family rate ratio is that a family rate is somewhat higher than it otherwise should be, and the single rate is somewhat lower that it otherwise should be.
Answer: A
NEW QUESTION 3
The following transactions occurred at the Lane Health Plan:
✑ Transaction 1 — Lane recorded a $25,000 premium prior to receiving the payment
✑ Transaction 2 — Lane purchased $500 in office expenses on account, but did not record the expense until it received the bill a month later
✑ Transaction 3 — Fire destroyed one of Lane’s facilities; Lane waited until the facility was rebuilt before assessing and recording the amount of loss
✑ Transaction 4 — Lane sold an investment on which it realized a $14,000 gain; Lane recorded the gain only after the sale was completed.
Of these transactions, the one that is consistent with the accounting principle of conservatism is:
- A. Transaction 1
- B. Transaction 2
- C. Transaction 3
- D. Transaction 4
Answer: D
NEW QUESTION 4
If the operational budget prepared by the Satilla health plan is typical of most operational budgets, then
- A. Its purpose is to track Satilla's operations and short-term profitability
- B. The key information source for this operational budget is Satilla's external environment
- C. The time frame for this operational budget is three to five years
- D. Its focus is on the threats that Satilla faces from its external environment
Answer: A
NEW QUESTION 5
Many clinicians are concerned about the development of practice guidelines that seek to define appropriate healthcare services that should be provided to a patient who has been diagnosed with a specific condition. To avoid the risk associated with using such guidelines, health plans should advise clinicians that the existence of such a guideline:
* 1. Establishes standards of care to be routinely utilized with all patients presenting a specific condition
* 2. Preempts a physician’s judgment when assessing the specific factors related to a patient’s condition
- A. Both 1 and 2
- B. 1 only
- C. 2 only
- D. Neither 1 nor 2
Answer: D
NEW QUESTION 6
The methods of alternative funding for health coverage can be divided into the following general categories:
✑ Category A—Those methods that primarily modify traditional fully insured group insurance contracts
✑ Category B—Those methods that have either partial or total self funding
Typically, small employers are able to use some of the alternative funding methods in
- A. Both Category A and Category B
- B. Category A only
- C. Category B only
- D. Neither Category A nor Category B
Answer: C
NEW QUESTION 7
The traditional financial ratios that analysts use to study a health plan's GAAP-based financial statements include liquidity ratios, activity ratios, leverage ratios, and profitability ratios. Of these categories of ratios, analysts are most likely to use
- A. Liquidity ratios to measure a health plan's ability to meet its current liabilities
- B. Activity ratios relate the returns of a health plan to its sales, total revenues, assets, stockholders' equity, capital, surplus, or stock share price
- C. Leverage ratios to measure how quickly a health plan converts specified financial statement items into premium income or cash
- D. Profitability ratios to measure the effect that fixed costs have on magnifying a health plan's risk and return
Answer: A
NEW QUESTION 8
With regard to the financial statements prepared by health plans, it can correctly be stated that
- A. both for-profit, publicly owned health plans and not-for-profit health plans are required by law to provide all interested parties with an annual report
- B. a health plan's annual report typically includes an independent auditor's report and notes to the financial statements
- C. any health plan that owns more than 20% of the stock of a subsidiary company must compile the financial statements for the health plan's annual report on a consolidated basis
- D. a health plan typically must prepare the financial statements included in its annual report according to SAP
Answer: B
NEW QUESTION 9
The following statements are about risk management in health plans. Select the answer choice containing the correct response.
- A. Risk management is especially important to health plans because the Employee Retirement Income Security Act of 1974 (ERISA) allows plan members to recover punitive damages from healthcare plans.
- B. With regard to the relative risk for health plan structures based upon the degree of influence and relationships that health plans maintain with their providers, preferred provider organizations (PPOs) typically have a higher risk than do group HMOs and staff HMOs.
- C. Although there are clear risks associated with the provision of healthcare services and coverage decisions surrounding that care, the bulk of risk in health plans is associated with a health plan's benefit administration and contracting activities.
- D. A health plan generally structures its risk management process around loss reduction techniques and loss transfer techniques.
Answer: D
NEW QUESTION 10
Most organizations that obtain group healthcare coverage can be classified as one of three types of groups: employer-employee groups, multiple employer groups, and professional associations. One true statement about these types of groups is that
- A. Anti selection risk is higher for both multiple-employer groups and professional associations than it is for an employer-employee group
- B. Private employers typically present a higher underwriting risk to health plans than do public employers
- C. Individual members of a multiple-employer group or a professional association typically are required to obtain healthcare coverage through the group or association
- D. I health plan is prohibited, when evaluating the risks represented by a professional association, from considering the industry experience of the agent or broker that sells a group plan to the association
Answer: A
NEW QUESTION 11
The following statements indicate the pricing policies of two health plans that operate in a particular market:
✑ The Accent Health Plan consistently underprices its product
✑ The Bolton Health Plan uses extremely strict underwriting practices for the small groups to which it markets its plan
From the following answer choices, select the response that correctly indicates the most likely market effects of the pricing policies used by Accent and Bolton.
- A. Accent = unprofitable business Bolton = high acquisition rate
- B. Accent = unprofitable business Bolton = low acquisition rate
- C. Accent = high profits Bolton = high acquisition rate
- D. Accent = high profits Bolton = low acquisition rate
Answer: B
NEW QUESTION 12
The types of financial risks and costs to which a health plan is subject depends on whether the health plan provides services to the Medicare and/or Medicaid populations or to the commercial population. One distinction between providing services to the Medicare and Medicaid populations and to the commercial population is that Medicare and Medicaid enrollees typically:
- A. Are locked into a plan for a 12-month period, whereas enrollees from the commercial population may disenroll from a plan on a monthly basis
- B. Require less enrollee education than do enrollees from the commercial population
- C. Have higher incidences of chronic illness than do enrollees from the commercial population
- D. Are enrolled in a health plan through a group situation, whereas the commercial population typically enrolls in a health plan on an individual basis
Answer: C
NEW QUESTION 13
The accounting department of the Enterprise health plan adheres to the following policies:
✑ Policy A—Report gains only after they actually occur
✑ Policy B—Report losses immediately
✑ Policy C—Record expenses only when they are certain
✑ Policy D—Record revenues only when they are certain
Of these Enterprise policies, the ones that are consistent with the accounting principle of conservatism are Policies
- A. A, B, C, and D
- B. A, B, and D only
- C. A and B only
- D. C and D only
Answer: B
NEW QUESTION 14
Contingency risks, or C-risks, are general categories of risk that have a direct bearing on both the cash flow and solvency of a health plan. One of these C-risks, pricing risk (C-2 risk), is typically the most important risk a health plan faces. Pricing risk is crucial to a health plan’s solvency because:
- A. A sizable portion of any health plan’s assets are held in long-term investments and anyshift in interest rates can significantly impact a health plan’s ability to pay medical benefits
- B. A health plan relies heavily on the sound judgment of its management, and poor management decisions can result in financial losses for the health plan
- C. A situation in which actual expenses exceed the amounts budgeted for those expenses may result in the health plan failing to retain assets sufficient to cover current obligations
- D. A sizable portion of the total expenses and liabilities faced by a health plan come from contractual obligations to pay future medical costs, and the exact amounts of those costs are not known at the time a product’s premium is established
Answer: D
NEW QUESTION 15
The risk-based capital formula for health plans defines a number of risks that can impact a health plan’s solvency. These categories reflect the fact that the level of risk faced by health plans is significantly impacted by provider reimbursement methods that shift utilization risk to providers. The following statements are about the effect of a health plan transferring utilization risk to providers. Select the answer choice containing the correct statement:
- A. The net effect of using provider reimbursement contracts to transfer risk is that the health plan’s net worth requirement increases.
- B. Once the health plan has transferred utilization risk to its providers, it is relieved of the legal obligation to provide medical services to plan members in the event of the provider’s insolvency.
- C. The greater the amount of risk the health plan transfers to providers, the larger the credit-risk factor becomes in the health plan’s RBC formula.
- D. By decreasing its utilization risk, the health plan increases its underwriting risk.
Answer: C
NEW QUESTION 16
The following statements illustrate the use of different rating methods by health plans:
✑ The Dover health plan established rates for small groups by using a rating method which requires that the average premium in each group cannot be more than 120% of the average premium for any other group. Under this method, all members of each group pay the same premium, which is based on the experience of the group.
✑ Under the rating method used by the Rolling Hills health plan, the health plan
calculates the ratio of a group's experience to the group's historical manual rate. Rolling Hills then multiplies this ratio by the group's future manual rate. Rolling Hills cannot consider the group's experience in determining premium rates.
From the following answer choices, select the response that correctly indicates the rating methods used by Dover and Rolling Hills.
- A. Dover = modified community rating Rolling Hills = factored rating
- B. Dover = modified community rating Rolling Hills = adjusted community rating (ACR)
- C. Dover = community rating by class (CRC) Rolling Hills = factored rating
- D. Dover = community rating by class (CRC) Rolling Hills = adjusted community rating (ACR)
Answer: D
NEW QUESTION 17
......
P.S. Certshared now are offering 100% pass ensure AHM-520 dumps! All AHM-520 exam questions have been updated with correct answers: https://www.certshared.com/exam/AHM-520/ (215 New Questions)