How Many Questions Of AHM-520 Test Preparation
It is more faster and easier to pass the AHIP AHM-520 exam by using Simulation AHIP Health Plan Finance and Risk Management questuins and answers. Immediate access to the Update AHM-520 Exam and find the same core area AHM-520 questions with professionally verified answers, then PASS your exam with a high score now.
Online AHIP AHM-520 free dumps demo Below:
NEW QUESTION 1
Costs that can be defined by behavior are most commonly classified as fixed costs, variable costs and semi-variable costs. Examples of fixed costs include:
- A. Rent, insurance expense, and depreciation on computer equipment
- B. Rent, claims processing costs, and selling expenses
- C. Claims processing costs, telephone expense, and depreciation on computer equipment
- D. Premium processing, rent, and selling expenses
Answer: A
NEW QUESTION 2
One way that a health plan can protect itself against case stripping is by requiring:
- A. Employees covered by a small group plan to contribute 100% of the cost of the healthcare coverage
- B. The small group to have no more than 10 members
- C. A minimum level of participation in order for a small group to be eligible for healthcare coverage
- D. Its underwriters to consider the characteristics of the employer, but not of the group members, when underwriting the group
Answer: C
NEW QUESTION 3
The Acorn Health Plan uses a resource-based relative value scale (RBRVS) to help determine the reimbursement amounts that Acorn should make to providers who are compensated under an FFS system. With regard to the advantages and disadvantages to Acorn of using RBRVS, it can correctly be stated that
- A. An advantage of using RBRVS is that it can assist Acorn in developing reimbursement schedules for various types of providers in a comprehensive healthcare plan
- B. An advantage of using RBRVS is that it puts providers who render more medical services than necessary at financial risk for this overutilization
- C. A disadvantage of using RBRVS is that it will be difficult for Acorn to track treatment rates for the health plan's quality and cost management functions
- D. A disadvantage of using RBRVS is that it rewards procedural healthcare services more than cognitive healthcare services
Answer: A
NEW QUESTION 4
A health plan can use cost accounting in order to
- A. Determine premium rates for its products
- B. Match the costs incurred during a given accounting period to the income earned in, or attributed to, that same period
- C. Both A and B
- D. A only
- E. B only
- F. Neither A nor B
Answer: A
NEW QUESTION 5
Provider reimbursement methods that transfer some utilization risk from a health plan to providers affect the health plan's RBC formula. A health plan's use of these reimbursement methods is likely to result in
- A. An increase the health plan's underwriting risk
- B. A decrease the health plan's credit risk
- C. A decrease the health plan's net worth requirement
- D. All of the above
Answer: C
NEW QUESTION 6
Mandated benefit laws are state or federal laws that require health plans to arrange for the financing and delivery of particular benefits. Within a market, the implementation of mandated benefit laws is likely to cause _______.
- A. A reduction in the number of self-funded healthcare plans
- B. An increase in the cost to the health plans
- C. A reduction in the size of the provider panels of health plans
- D. A reduction in the uniformity among the healthcare plans of competing health plans
Answer: B
NEW QUESTION 7
The Puma health plan uses return on investment (ROI) and residual income (RI) to measure the performance of its investment centers. Two of these investment centers are identified as X and Y. Investment Center X earns $10,000,000 in operating income on controllable investments of $50,000,000, and it has total revenues of $60,000,000. Investment Center Y earns $2,000,000 in operating income on controllable investments of $8,000,000, and it has total revenues of $10,000,000. Both centers have a minimum required rate of return of 15%.
The following statements are about Puma's evaluation of these investment centers. Select the answer choice containing the correct statement.
- A. Investment Center Y's RI is greater than Investment Center X's RI.
- B. The ROI for Investment Center X is 16.7%, and the ROI for Investment Center Y is 20.0%.
- C. Because Investment Centers X and Y are different sizes, Puma should not use ROI to compare these investment centers.
- D. According to the evaluation of ROI, Investment Center Y achieves a higher return on its available resources than does Investment Center X.
Answer: D
NEW QUESTION 8
An investor deposited $1,000 in an interest-bearing account today. That sum will accumulate to $1,200 two years from now. One true statement about this transaction is that:
- A. The process by which the original $1,000 deposit grows to $1,200 is known as compounding
- B. $1,200 is the present value of the $1,000 deposit
- C. The $200 increase in the deposit’s value is its incremental cash flow
- D. The $200 difference between the original deposit and the accumulated value of the deposit is known as the deposit’s discount
Answer: A
NEW QUESTION 9
In order to print all of its forms in-house, the Prism health plan is considering the purchase of 10 new printers at a total cost of $30,000. Prism estimates that the proposed printers have a useful life of 5 years. Under its current system, Prism spends $10,000 a year to have forms printed by a local printing company. Assume that Prism selects a 15% discount rate based on its weighted-average costs of capital. The cash inflows for each year, discounted to their present value, are shown in the following chart: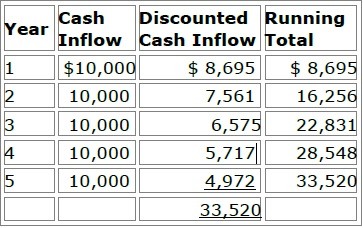
Prism will use both the payback method and the discounted payback methodto analyze the worthiness of this potential capital investment. Prism's decisionrule is to accept all proposed capital projects that have payback periods offour years or less.
After analyzing this information, Prism would accept this proposed capitalproject under
- A. Both the payback method and the discounted payback method
- B. The payback method but not the discounted payback method
- C. The discounted payback method but not the payback method
- D. Neither the payback method nor the discounted payback method
Answer: B
NEW QUESTION 10
In the following paragraph, a sentence contains two pairs of words enclosed in parentheses. Determine which word in each pair correctly completes the statement. Then select the answer choice containing the two words that you have selected.
The Igloo health plan recognizes the receipt of its premium income during the accounting
period in which the income is earned, regardless of when cash changes hands. However, Igloo recognizes its expenses when it earns the revenues related to those expenses, regardless of when it receives cash for the revenues earned. This information indicates that the (realization/capitalization) principle governs Igloo's revenue recognition, whereas the (matching/initial-recording) principle governs its expense recognition.
- A. realization / matching
- B. realization / initial-recording
- C. capitalization / matching
- D. capitalization / initial-recording
Answer: A
NEW QUESTION 11
All publicly traded health plans in the United States are required to prepare financial statements for use by their external users in accordance with generally accepted accounting principles (GAAP). In addition, health insurers and health plans that fall under the jurisdiction of state insurance departments are required by law to prepare certain financial statements in accordance with statutory accounting practices (SAP). In a comparison of GAAP to SAP, it is correct to say that:
- A. GAAP is established and promoted by the National Association of Insurance Commissioners (NAIC), whereas SAP is established and promoted by the Financial Accounting Standards Board (FASB)
- B. The going-concern concept is an underlying premise of GAAP, whereas SAP tends to focus on the liquidation value of the MCO or the insurer
- C. GAAP provides for a single method of valuing all of a health plan’s assets, whereas SAP offers the health plan more than one method for valuing its assets
- D. The principle of conservatism is fundamental to GAAP, whereas SAP generally is not conservative in nature
Answer: B
NEW QUESTION 12
The following information relates to the Hardcastle Health Plan for the month of June:
✑ Incurred claims (paid and IBNR) equal $100,000
✑ Earned premiums equal $120,000
✑ Paid claims, excluding IBNR, equal $80,000
✑ Total health plan expenses equal $300,000
This information indicates that Hardcastle’s medical loss ratio (MLR) for the month of June was approximately equal to:
- A. 40%
- B. 67%
- C. 83%
- D. 120%
Answer: C
NEW QUESTION 13
In order to analyze costs for internal management purposes, the Banner health plan uses functional cost analysis. One characteristic of this method of cost analysis is that it
- A. Enables Banner's top management to analyze costs as they apply to workflow rather than to organizational structures
- B. Assumes that activities, not products, generate costs
- C. Cannot be used when Banner makes pricing and staffing decisions
- D. Identifies units of activity, calculates the costs of performing each unit of activity, and then assigns the cost of each unit of activity to Banner's products or lines of business
Answer: A
NEW QUESTION 14
Health plans with risk-based Medicare contracts are required to calculate and submit to CMS a Medicare adjusted community rate (Medicare ACR). Medicare ACR can be defined as the:
- A. Estimated cost of providing services to a beneficiary under Medicare FFS, adjusted for factors such as age and gender
- B. Health plan’s estimate of the premium it would charge Medicare enrollees in the absence of Medicare payments to the health plan
- C. Average amount the health plan expects to receive from CMS per beneficiary covered
- D. Health plan’s actual costs of providing benefits to Medicare enrollees in a given year
Answer: B
NEW QUESTION 15
A financial analyst wants to learn the following information about the Forest health plan for a given financial period:
- A. Forest's beginning-of-period cash balance
- B. Forest's minimum cash balance
- C. The cash needs of Forest during the period
- D. Forest's end-of-period cash balanceFrom Forest's cash budget, the analyst most likely can obtain information about
- E. A, B, C, and D
- F. A, B, and C only
- G. A and D only
- H. B and C only
Answer: A
NEW QUESTION 16
In order to achieve its goal of improved customer service, the Evergreen Health Plan will add three new customer service representatives to its existing staff, install a new switching station, and install additional phone lines. In this situation, the cost that would be classified as a sunk cost, rather than a differential cost, is the expense associated with:
- A. Adding new customer service representatives
- B. Maintaining the existing staff
- C. Installing a new switching station
- D. Installing additional phone lines
Answer: B
NEW QUESTION 17
......
P.S. 2passeasy now are offering 100% pass ensure AHM-520 dumps! All AHM-520 exam questions have been updated with correct answers: https://www.2passeasy.com/dumps/AHM-520/ (215 New Questions)